Study findings published in Oncotarget show specific genetic predictors of cardiotoxicity in patients treated with the Bruton tyrosine kinase (BTK) inhibitor ibrutinib, the first BTK inhibitor approved for the treatment of chronic lymphocytic leukemia. Researchers have discovered that specific single nucleotide polymorphisms (SNPs) in DONE4 AND KCNQ1 genes are associated with a higher probability of cardiovascular events.1
The study, conducted by researchers from Atrium Health Levine Cancer Institute and Baptist Atrium Health Wake Forest Comprehensive Cancer Center, identified 3 SNPs significantly associated with ibrutinib-related cardiovascular events: GATA4 rs804280, KCNQ1 rs163182, and KCNQ1 rs163182, and K25C .2 Using a next-generation sequencing panel to genotype 40 SNPs, the researchers found that a high genetic risk score, defined as the presence of at least 2 of these genotypes, was associated with an 11.5-fold increased risk of cardiovascular events.P = .019; 95% CI, 1.79119.73).
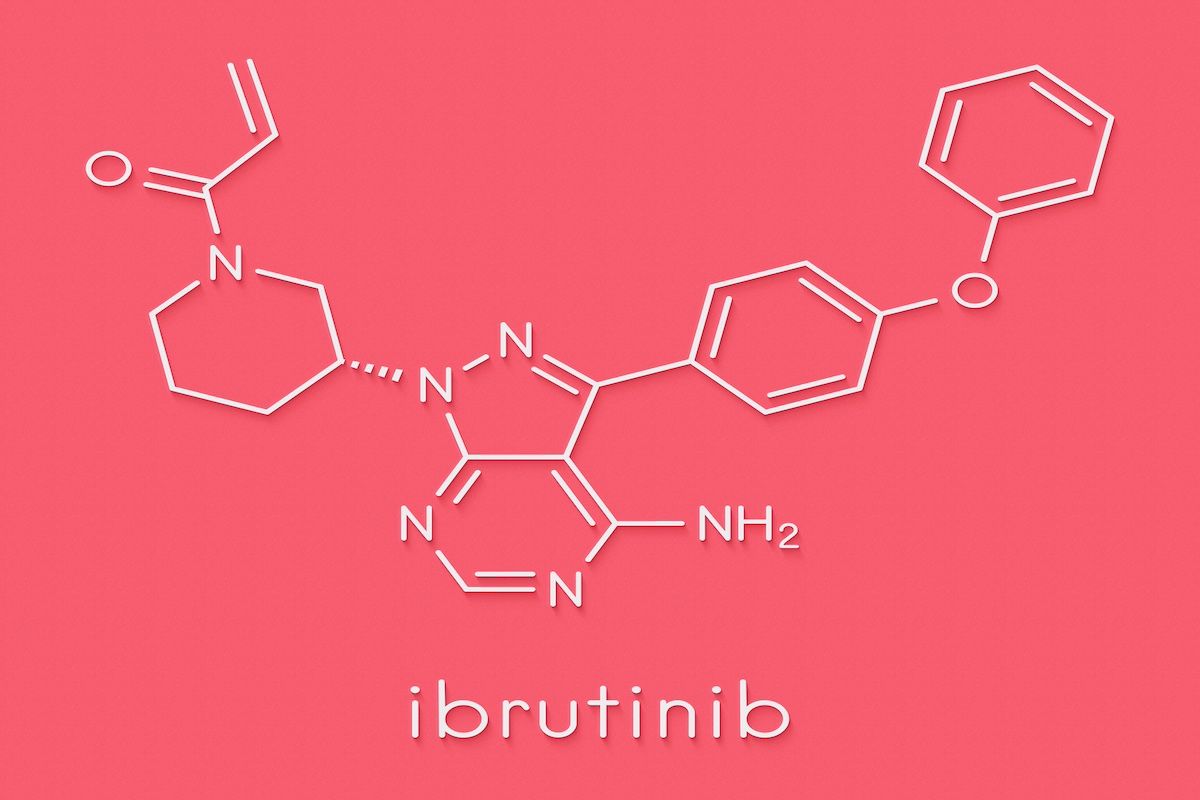
The FDA first approved ibrutinib in November 2013 to treat mantle cell lymphoma, and today it has 5 indications for hematologic cancer| Image credit: molekuul.be-stock.adobe.com
Their study findings show that treatment with ibrutinib increased the incidence of severe hypertension by 3-fold and atrial fibrillation by more than 4-fold.3 Real-world data indicate that approximately 20% to 25% of patients experience these dose-limiting cardiovascular toxicities, leading to higher discontinuation rates. Current clinical predictors of cardiotoxicity associated with BTK inhibitors include age greater than 65 years, history of atrial fibrillation, heart failure, and left atrial abnormalities. The development of adverse cardiovascular effects associated with BTK inhibitors is associated with worse overall survival.4
Current recommendations from an international consensus group for the screening and management of cardiotoxicity associated with BTK inhibitors are also discussed. The group recommends a comprehensive pretreatment workup, including a detailed, comprehensive history, medication reconciliation, cardiovascular risk assessment, and screening (including electrocardiogram in high-risk patients) prior to treatment. In addition, patients with cardiovascular risk factors should be referred to a cardio-oncologist before starting BTK inhibitor treatment to ensure that cardiovascular disease is adequately managed. Any adverse cardiovascular effects that develop should be diagnosed quickly, and a multidisciplinary approach, including a hematologist and cardio-oncologist, should be used to evaluate the risks versus benefits of continuing BTK inhibitor therapy.
The authors note, “A combined clinical and genetic BTK inhibitor cardiotoxicity risk model that outperforms current clinical risk models would be ideal in personalized, multidisciplinary care with a focus on high specificity, good sensitivity, and a degree of low misclassification”.
For patients without cardiovascular risk factors, any approved BTK inhibitor may be appropriate. However, for those with existing risk factors, more selective drugs such as akalabrutinib or zanubrutinib should be considered. The frequency of monitoring should be appropriate for the patient’s risk during treatment. The use of BTK inhibitors is not recommended in patients with a history of ventricular arrhythmia, family history of sudden cardiac death, severe uncontrolled hypertension, or severe or uncontrolled congestive heart failure.
The authors conclude by calling for the development and validation of a clinicogenomic algorithm for risk stratification of cardiovascular events in patients receiving BTK inhibitors.
“There is a great need for the development and validation of a clinicogenomic algorithm for [cardiovascular side effect] risk stratification and future studies evaluating the clinical utility of such an algorithm to test different risk mitigation strategies. This would enable a more personalized approach to the selection of anticancer treatments, CV monitoring, [and] implementation of pharmacological or non-pharmacological interventions, all with the hope of improving the survival of cancer patients.”
References
1. Patel JN, Singh J, Ghosh N. Bruton’s tyrosine kinase inhibitor-associated cardiotoxicity: Search for predictive biomarkers and improved risk stratification. Oncotarget. 2024; 15: 355-359. Published June 3, 2024. doi:10.18632/oncotarget.28589
2. Hamadeh IS, Patel JN, Jacobs R, et al. Genetic predictors of ibrutinib-related cardiovascular side effects in patients with chronic lymphocytic leukemia. Clin Cancer Res. 2023; 29 (23): 4941-4948. doi: 10.1158/1078-0432.CCR-23-0421
3. Caldeira D, Alves D, Costa J, et al. Ibrutinib increases the risk of hypertension and atrial fibrillation: Systematic review and meta-analysis. PLoS One. 2019; 14 (2): e0211228. doi:10.1371/journal.pone.0211228
4. Parikh P, Aggarwal IB, Daddi A, et al. Ibrutinib and atrial fibrillation as cardiotoxicity – A new safety warning affecting overall survival. Int J Mol Immuno Oncol. 2022; 7:54-57. doi: 10.25259/IJMIO_1_2022
#Study #reveals #genetic #markers #BTK #inhibitorrelated #cardiotoxicity
Image Source : www.ajmc.com